GERD Symptoms, Treatment, Causes, Diet & More
Gastroesophageal
reflux disease (GERD) is a condition where stomach acid flows back up from the
esophagus into the throat. It causes heartburn, chest pain, coughing,
hoarseness, sore throat, and other symptoms.
Learn
more about this common digestive disorder with our comprehensive article.
What Is GERD (Gastroesophageal Reflux Disease)?
A person with gastroesophageal reflux disease (GERD) has refluxed more than twice a week.
GERD can be dangerous if left untreated because the reflux of stomach acid damages the tissue lining the esophagus, causing inflammation and irritation. Long-term untreated GERD in adults can result in permanent esophageal damage.
Are GERD and acid reflux the same?
Acid reflux occurs when the contents
of your stomach, such as food or acids, flow backward. They pass from your
stomach to your throat via the tube that connects them, your esophagus.
You may taste food or stomach acid in the back of your mouth if you have acid reflux. This might be unpleasant and make you feel ill. Acid reflux is also known as GERD (gastroesophageal reflux).
GERD, as the name implies, is a more
severe form of acid reflux. They both have the potential to produce heartburn.
People who have heartburn more than twice a week are more likely to have GERD.
What Factors Contribute to GERD?
Acidic stomach contents reflux into the esophagus, resulting in GERD. The esophagus is a tube that connects the mouth to the stomach and carries food and liquids. It is separated from the stomach by a tiny muscle (the esophageal sphincter). This muscle opens to allow food and liquid into the stomach and closes to keep it from spilling back into the esophagus.
GERD occurs when a muscle relaxes at an inopportune time or fails to close properly.
This can occur for a number of reasons, including:
- Some people's muscles are not tense enough.
- In others, it fails to seal properly or at all, allowing stomach contents to wash back up.
- If a person overeats, the stomach muscles may become stretched and cease to function properly.
GERD, risk factors.
Nobody knows for sure what causes GERD. Doctors are aware that certain factors, such as weight, alcohol consumption, and pregnancy, can aggravate GERD.
Certain foods and medications may exacerbate GERD symptoms. Many people experience the following symptoms as a result of eating these foods:
GERD, foods to avoid
- Clementines
- Dark chocolate
- Caffeine-containing beverages or
foods
- Fried and greasy foods
- Onions with garlic
- Spearmint
- Hot foods
- Spaghetti sauce, chili, and pizza are all tomato-based dishes.
GERD types:
GERD is classified into stages based on how severe your symptoms are and how frequently they occur:
- Stage 1: Mild GERD
Once or twice a month, I experience
minor acid reflux. At this stage, GERD symptoms are usually manageable by
dietary and lifestyle adjustments, as well as over-the-counter acid reflux
medication if necessary.
- Stage 2: Moderate GERD
Symptoms are severe enough to
necessitate the use of acid reflux medication, which is normally taken daily.
GERD symptoms can interfere with daily activities.
- Stage 3: Severe GERD
Symptoms are painful at this stage
and may not improve even with prescribed treatment. Your quality of life is
suffering, and your doctor may propose surgical GERD treatment.
- Stage 4: Precancer or cancer
After years of untreated severe GERD
symptoms, the esophagus might develop Barrett's esophagus, a precancerous
condition. Without treatment, precancerous lesions might develop into
esophageal cancer.
What are the GERD symptoms?
The patient may complain of classic
reflux symptoms (heartburn and regurgitation) or not, in which case the reflux
is called silent reflux.
When food or liquid containing stomach acid is regurgitated into the esophagus or mouth, this is a symptom of GERD. However, regurgitation, like heartburn, is common in everyone.
Associated esophageal symptoms may
include:
Constant burping
Chest and abdominal pain
Frequent vomiting
Bad breath
Tooth decay and erosion
Ulcers in the mouth and gums
A sensation of a lump in the
esophagus that prevents swallowing and does not move despite continuous
swallowing
Persistent sore throat
Recurrent sinusitis and throat
secretions
Constant dry cough and stinging
The constant change of voice or hoarseness of voice
Continuous hem
The presence of a persistent taste
of bitterness, especially in the morning
The constant need to moisten the
throat
Difficulty breathing and swallowing
A feeling that food gets stuck in your throat
A feeling of choking that may wake
you up
Heart palpitations and GERD.
GERD frequently causes chest
tightness or a burning sensation in the chest. The burning feeling can cease
and restart, which can be painful.
The resumption of GERD can feel like
heart palpitations, but GERD is rarely the cause of palpitations. Patients with
GERD may experience palpitations because of the fear and anxiety of their
medical condition.
A heart palpitation happens when the
electrical rhythm of the heart is disrupted. Palpitations might feel like a
flutter in the chest as if the heart has skipped a beat and is racing to catch
up.
What are the complications of GERD?
• Bleeding because of ulcers in the
esophagus
• Narrowing in the esophagus and
difficulty swallowing because of fibrosis of the esophageal wall due to
continuous inflammation.
• Esophageal cancer: This may happen
in the long term because of the patient's neglect of treatment and continuous
medical follow-up.
Red flag signs of GERD
These signs, if it appears, it necessitates
an urgent doctor consultation
-Iron deficiency anemia
-Vomiting of blood or dark-colored
stool
- The difficulty of swallowing and not
responding to medications
-weight loss
How Is GERD Diagnosis Made?
If symptoms are persistent in spite of treatment, doctors may order some tests to diagnose GERD or rule out other possible problems:
- Upper endoscopy
Doctors examine the esophagus, stomach, and a portion of the small intestine with a tiny fiber-optic camera. They may also take a small tissue sample from the esophageal lining (a biopsy) to rule out or find other abnormalities like Barret's esophagus. Most patients are sedated and "asleep" during this treatment.
- 24-hour impedance-PH probe investigation.
This is the most accurate method of determining the frequency of reflux. Through the nose, a thin, flexible tube is inserted into the esophagus. The tip is placed slightly above the esophageal sphincter for 24 hours to monitor acid levels in the esophagus and detect any reflux.
Upper GI radiology study.
This specialized X-ray can detect liquid backing up into the esophagus, esophageal irritation or constriction, and any upper digestive system abnormalities. You will swallow a small amount of grainy liquid for the test (barium). This liquid is visible on the X-ray and represents the swallowing process.
Gastric emptying scan (milk scan)
This can help determine whether a
person's stomach is emptying too slowly, which can increase the likelihood of
reflux. This test is performed by either drinking tracer-laced milk or eating
tracer-laced scrambled eggs. A non-radioactive machine can detect the tracer
and determine where it goes and how quickly it empties the stomach.
How GERD is treated.
The severity of the symptoms determines GERD treatment. For some people, treatment may consist of simple lifestyle changes such as changing what they eat or drink. Others will be required to take medication. In very rare cases, when GERD is particularly severe, a doctor may recommend surgery.
Lifestyle changes:
These lifestyle changes can help alleviate or even prevent GERD symptoms:
- Quitting smoking
- Abstinence from alcohol
- Weight loss if you are overweight
- Consuming small meals
- Dressing in baggy clothes
- Avoiding carbonated beverages
- Avoiding foods that cause acid reflux
-It may also be beneficial to avoid lying down for three hours after eating and to avoid eating two to three hours before going to bed. Doctors may also recommend that you raise the head of your bed by 6 to 8 inches or use a reflux pillow.
If symptoms persist, doctors may
prescribe medications such as:
GERD medications:
-H2 blockers can help reduce stomach acid production.
- Proton pump inhibitors reduce the amount of acid produced by the stomach.
- Prokinetics, which improves esophageal sphincter function and allows the stomach to empty faster. This can help to prevent reflux attacks.
Surgery for Severe GERD
If you require regular high doses of PPIs to regulate your symptoms, have esophageal damage despite medication, and have a hiatal hernia, you may require GERD surgery. However, you should first exhaust all other options.
Fundoplication
It is a surgical treatment that raises the pressure in your esophagus. The top of your stomach will be wound around the LES by the doctor. This tightens the muscle and raises the pressure in your lower esophagus, which helps to prevent reflux. This will be done either through a laparoscope (small holes in the belly) or during open surgery.
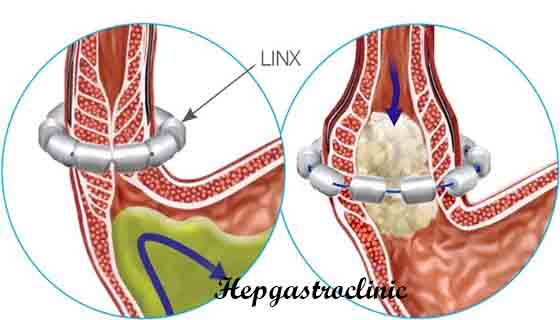
LINX surgery:
A band of magnetic titanium beads is wrapped all around the junction of your stomach and esophagus by your doctor. The magnetic attraction of the beads allows food to pass through while keeping them tight enough to avoid reflux.
Endoscopic treatment of GERD
This type of treatment is
accomplished by the gastroscope as an alternative to surgery, it includes:
Transoral incisionless fundoplication (TIF):
An endoscope (a small tube with a camera) is used in a newer version of this technique to wrap the stomach around the LES with plastic fasteners. It is less invasive than a traditional fundoplication.
Stretta procedure:
Your doctor will insert a tiny tube into your esophagus that will employ low-radiofrequency heat to remodel your LES.
Prevention of GERD
Aside from the lifestyle adjustments
listed above, the following changes may aid in the prevention of GERD:
- Eat small meals frequently.
- Limit your intake of huge meals.
- Stay upright after eating.
- Before going to bed, eat for at least 2-3 hours.
- Stop or reduce your smoking.
- Avoid intense activities
immediately after eating.
- If you are overweight, you should
lose weight.
- Avoid wearing clothing that is too tight around the abdomen.
- Sleep with your head slightly
lifted and at an angle.
Foods That Decrease Acid Reflux (GERD diet)
Eat fiber-rich foods
Which
prevents the individual from overeating
It
includes:
Whole grains include oatmeal, couscous, and brown rice.
Sweet
potatoes, carrots, and beets are examples of root vegetables.
green
foods including green beans, broccoli, and asparagus.
Eat astringent foods
Which
neutralizes the gastric acidity
Alkaline
meals consist of:
Bananas
Melons
Cauliflower\Fennel\Nuts
Eat Watery dishes
To dilute
gastric acid. Select foods like:
Soups
made with celery, cucumber, lettuce, and watermelon broth
Flavored
tea
Does milk aid with heartburn relief?
Milk is thought to relieve heartburn; however, not all types of milk are the same; full cream milk may increase gastric acidity due to its high fat content, which may increase gastric acid secretion; on the other hand, skimmed milk may buffer the gastric acidity and cause immediate relief of heartburn. Low-fat yoghurt may also help to relieve heartburn and contains a lot of probiotics (good bacteria).
Summary
Acid reflux is not a cause for
concern until it occurs frequently and becomes chronic. In this case, heartburn
could be a symptom of GERD.
GERD is a treatable condition. A
combination of lifestyle changes and medications is often enough to treat it.
However, it may cause significant problems if left untreated and could require
surgery. I hope I answered your questions and I leave you now with a subtitled video about the most recent techniques for the treatment of GERD.